What is CDH?
Congenital diaphragmatic hernia (CDH) is a birth condition that affects approximately 1 in 2,500 babies. It occurs when there is a hole in the diaphragm, the muscle that separates the chest from the abdomen. This defect allows abdominal organs, such as the stomach, intestines, and sometimes the liver, to move into the chest cavity, restricting lung growth.
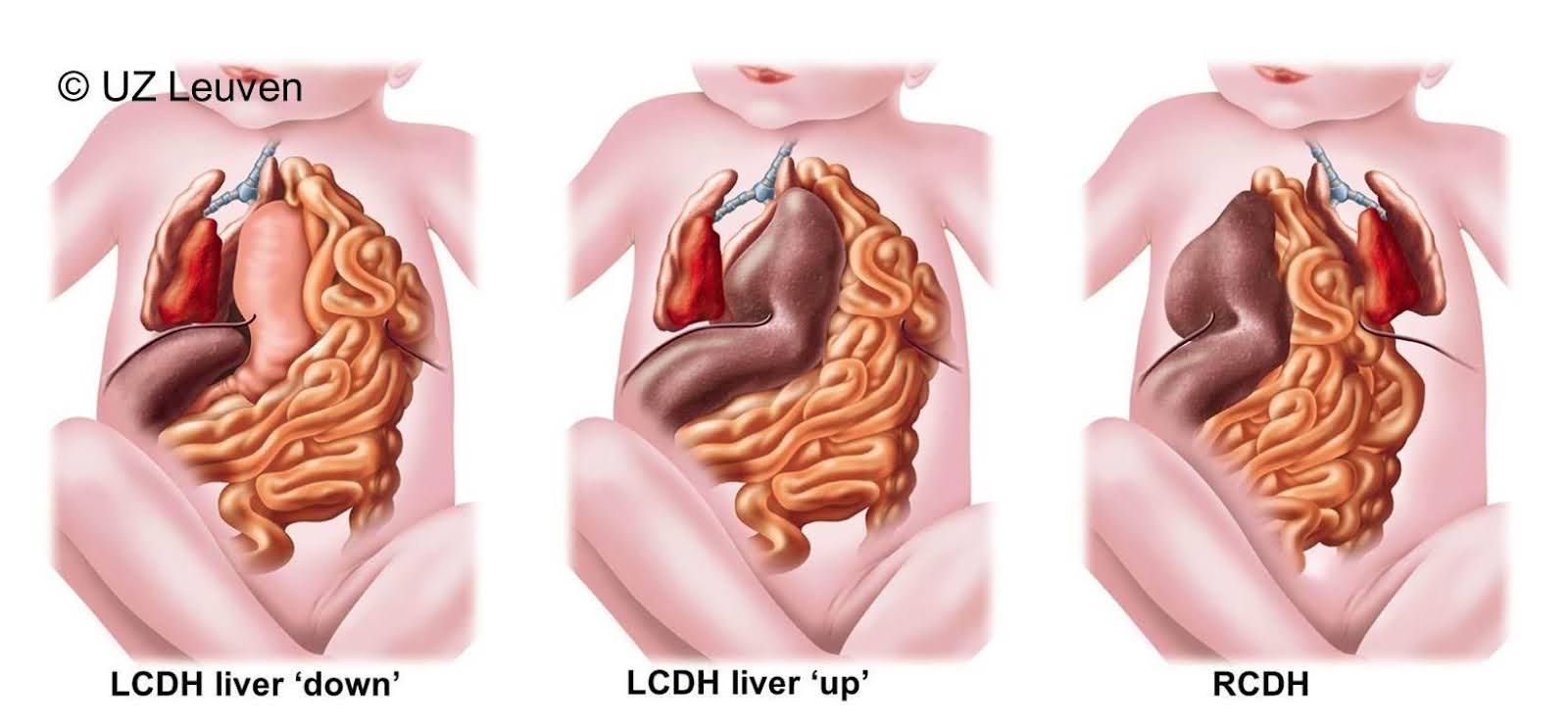
In over 80% of cases, the hole is on the left side of the diaphragm, around 20% on the right, and in very rare cases, it affects both sides. The condition develops early in pregnancy (around 8 weeks gestation), though the exact cause is often unknown.
CDH can occur on its own (isolated CDH) or as part of a broader genetic or chromosomal condition. Babies with additional medical conditions tend to have a poorer prognosis, whereas isolated CDH cases generally have better survival outcomes.
While CDH is typically diagnosed before birth, it can also occur later in life, including in adulthood, requiring surgery. However, the greatest challenge in newborns is not just r epairing the diaphragm but managing the impact of underdeveloped lungs (pulmonary hypoplasia) and high blood pressure in the lungs (pulmonary hypertension)before surgery can be performed.
the impact of cdh
The effects of CDH can be grouped into two stages:
- Before and at birth
- Long-term impacts on health
before and at birth
The biggest challenge in CDH is that lung growth is restricted before birth. Babies with CDH are often born with small, underdeveloped lungs, particularly on the affected side. These lungs have less elasticity, fewer airways, and a reduced ability to exchange oxygen.
During pregnancy, this isn't an issue because the baby receives oxygen through the placenta. However, once born, the baby must breathe on their own, which can be difficult due to:
- Severely underdeveloped lungs
- High blood pressure in the lungs (pulmonary hypertension)
- Displacement of abdominal organs into the chest cavity
As a result, CDH babies typically require immediate respiratory support at birth, often with ventilators, medications, and sometimes ECMO (a heart-lung bypass machine).
Once the baby is stable, surgery is performed within the first 10 days to repair the diaphragm. The gap is either stitched closed or, if too large, a patch is used to cover the defect. After surgery, the lungs may continue to grow, but their function is often still reduced.
Survival rates vary depending on lung size and access to specialised care. In optimal conditions, survival rates are improving, but worldwide, up to 30% of babies with isolated CDH do not survive the early weeks of life.
long term outcomes
Most children with CDH lead relatively normal lives, but some may face ongoing health challenges, including:
- Breathing difficulties – Some children have reduced lung function, affecting exercise capacity and increasing the risk of asthma or lung infections.
- Feeding problems – Many babies experience reflux due to stomach displacement, which may require medication or surgery.
- Growth and development – Some babies struggle with weight gain in infancy but catch up later.
- Spinal problems (scoliosis) – The chest wall may grow unevenly, leading to curvature of the spine.
- Hearing loss – For unknown reasons, some children with CDH develop hearing issues.
With appropriate follow-up care, most of these challenges can be managed.
Diagnosing and Managing CDH in Australia
CDH is usually detected during a routine pregnancy ultrasound. Receiving this diagnosis can be overwhelming for parents, so it is essential to be referred to a specialised centre with experience in managing CDH pregnancies and newborn care.
In Australia, this often means referral to a tertiary hospital with a neonatal intensive care unit (NICU) and paediatric surgery team. This may mean relocating from your home to a place where your baby can be cared for after birth. Specialist care may include:
- Fetal medicine assessment – To determine if CDH is isolated or linked to other conditions.
- Ultrasound & MRI scans – To measure lung size and liver position, helping predict the baby's prognosis.
- Genetic testing – In some cases, additional testing may be recommended to rule out genetic conditions.
While making decisions about the pregnancy, and planning birth, parents will have the opportunity to meet with a multidisciplinary team, including:
- Fetal medicine specialists (experts in high-risk pregnancies)
- Obstetricians (managing the pregnancy and birth)
- Neonatologists (specialists in newborn intensive care)
- Paediatric surgeons (who will perform the diaphragm repair surgery).
These specialists will guide parents through the diagnosis, prognosis, and treatment options before and after birth.
Predicting CDH Severity Before Birth
Doctors can estimate a baby’s chances of survival based on:
- Lung size – Measured using the Lung-to-Head Ratio (LHR) on ultrasound.
- Liver position – If the liver has moved into the chest, the condition is often more severe.
Using these factors, specialists classify CDH into three groups:
- Severe CDH – High risk, with low survival rates even with intensive care.
- Moderate CDH – 40-60% survival, with some long-term breathing difficulties.
- Mild CDH – 60-95% survival, with minimal ongoing issues.
Planning for Birth
Babies with CDH must be born in a hospital with a NICU to ensure they receive immediate breathing support.
- Most babies are delivered at around 38 weeks unless other complications arise.
- Vaginal birth or caesarean? There is no clear advantage to either mode, but the timing and hospital setting are carefully planned to ensure the best possible outcome.




